Hospitals across the US – including in the Great Plains, the Midwest and the Southwest – are seeing record highs of COVID-19 patients.
As of today, more than 44,000 people were hospitalized as the country deals with a third wave of the coronavirus pandemic, according to The COVID Tracking Project.
These are levels not seen since mid-August.
Some hospitals have reached maximum capacity and are setting up field hospitals to deal with the overflow while others report few available ICU beds.
And, in the most dire cases, medical care professionals have to determine which critically ill patients will get life-saving medical care and which will not.
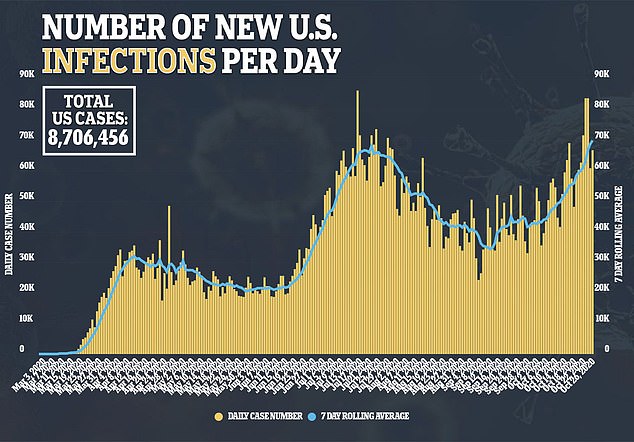
Over the weekend, the US recorded more than 83,000 new COVID-19 infections on both Saturday and Sunday – more than ever before.
Deaths – which were in the low 900s – also increased to their highest levels since September.
The Washington Post reports that 41 US states, and Puerto Rico, currently have more coronavirus patients hospitalized than they did at the end of September.
What’s more, half of those states have seen spikes of more than 50 percent in the number of people with COVID-19 who need inpatient care.
‘The data is just going up on hospitalizations,’ Ross McKinney, chief scientific officer of the Association of American Medical Colleges, told The Post.
‘And we are going to run into trouble, – it looks like – almost inevitably.’
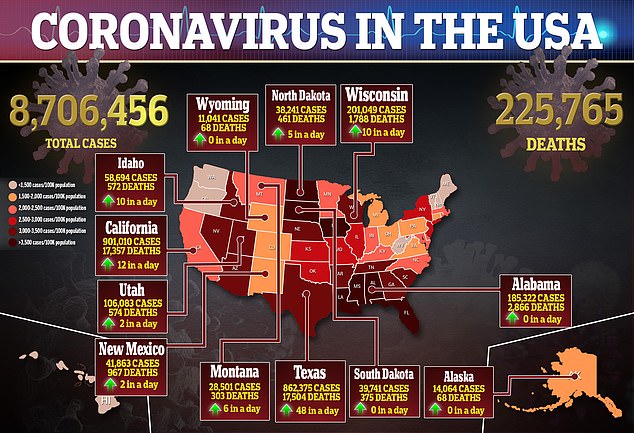
In El Paso, Texas, residents have been asked to stay home for two weeks after the border city recorded a more than 300 percent increase in hospitalizations in less that one month.
According to the city’s director of public health, Angel Mora, the number of hospitalizations over in the last three weeks has spiked from 259 to 786.
Hospitals and intensive care units are at 100 percent capacity and El Paso has 15 percent of all hospitalized COVID-19 patients in Texas, despite accounting for less than three percent of the state’s population.
To deal with the overflow, the city is turning its convention center into a field hospital with as many as 100 beds.
‘If we continue on this trend, we risk detrimental effects to our entire health care system,’ Mora said.
‘For the sake of those hospitalized and the front line health care workers working tirelessly each day to care for them, we ask you to please stay home for two weeks and eliminate your interactions with those outside your household until we can flatten the curve.’
In Utah, hospitalizations have ticked up, reaching as high as 300 for the first time ever earlier this month.
According to the state’s health department, ICU bed occupancy is currently at 76 percent, below the goal of 72 percent.
Greg Bell, the president of Utah’s hospital association, has warned that the state may reach its maximum occupancy for intensive care unit beds within two weeks.
He has met with Utah Gov Gary Herbert to discuss the Crisis Standards of Care Guidelines to determine – if need be – which patients may be denied critical care for those who could have better outcomes.
For example, the document recommends that ICU and ventilator be saved for those ‘that are more likely to benefit from it.’
‘We just know that hospitalizations follow [the] disease, and so we have to think in the next week or two that we’re going to be at the maximum of even our contingency planning for ICU beds,’ Bell told KSL.
In the Upper Midwest, hospitalizations are also surging.
North Dakota currently has 173 coronavirus patients hospitalized and there is a shortage of available hospital beds.
There are are only 20 available ICU beds and 123 regular, inpatient beds across the entire state, according to the latest figures.
Meanwhile, in Ohio, there are currently 1,456 COVID-19 patients hospitalized, which is a record-high since the pandemic began.
The Post reported that eight other states also set records on Monday: Iowa, Kentucky, Minnesota, Montana, New Mexico, South Dakota, West Virginia and Wisconsin.
In all regions of Michigan, hospitalizations have spiked by more than 80 percent over the last few weeks, according to WWMT.
Some hospitals ‘are being inundated with patients,’ Gary Roth, chief medical officer of the Michigan Health and Hospital Association, told The Post.
‘Are we getting concerned regarding the increasing numbers, the surging of patients coming into the hospitals? Absolutely.’